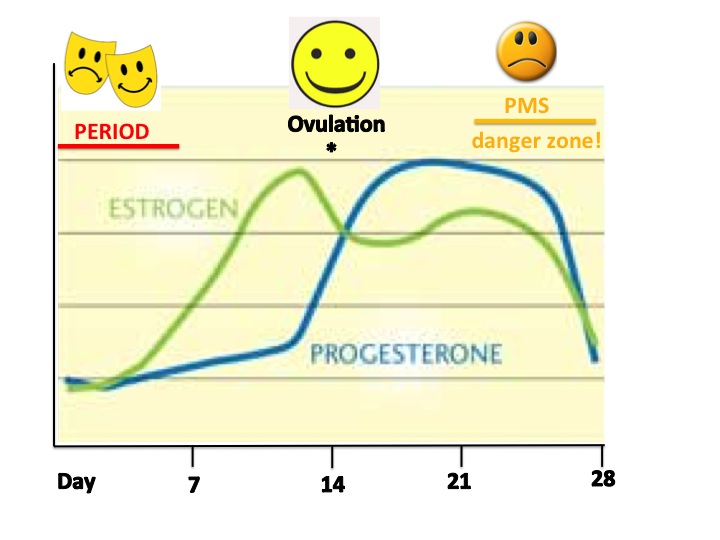
Some women have it easy both for PMS as well as for the rollercoaster that perimenopause can be, physically and emotionally. For those of us not so lucky, knowing the causes may bring some AHA moments and perhaps better ways to deal with the symptoms. In both cases, symptoms experienced are mainly due to hormone levels fluctuating. The main hormones are estrogen and progesterone (both produced in the ovaries; estrogen is produced in response to other hormones (FSH and LH) that stimulate the ovaries to do so, produced by the pituitary gland in the brain), which go up and down periodically in a monthly (lunar) fashion to result in our menstrual cycles or periods, as shown in the figure. Progesterone, produced in the ovary after ovulation, starts preparing the uterus for a fertilized egg, making it thicker with increased blood supply. If fertilization or implantation do not occur, the egg disintegrates and levels of estrogen and progesterone drop and the uterus contracts and period (bleeding) comes. It is the sudden drop in progesterone that occurs right before we bleed which causes many PMS symptoms.
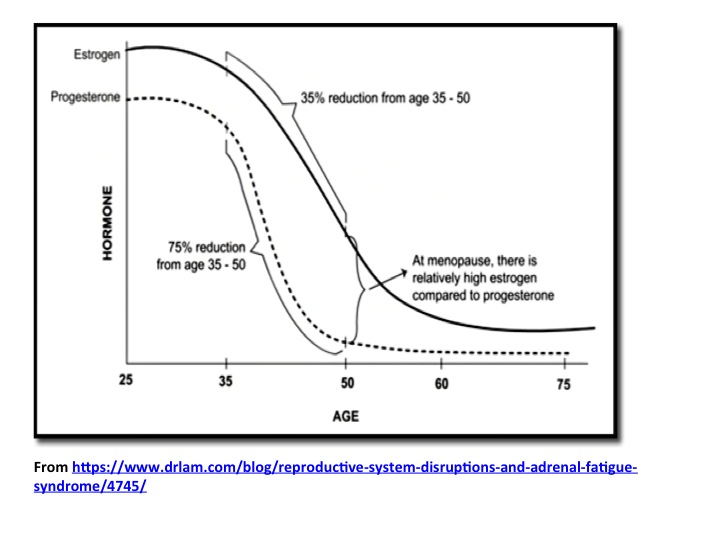
Perimenopause can start as early as late 30s or early 40s, while menopause (defined as 12 months or more without periods) occurs in average when women are around 51-52 years old. So if you do the math, perimenopause in some women can last up to 10 years, while others do not experience any major symptoms or they do for a much shorter time. The average time is 3-4 years. This "condition" is a transition due to hormone levels, although in this case is rather due to proportional levels of estrogen and progesterone (one compared to the other). A condition known as estrogen dominance, in which the drop in estrogen is small compared to the drop in progesterone, usually occurs in perimenopause and as a result there is a relative increase of estrogen in the body when compared to progesterone levels, all while the levels of these two hormones are generally declining during the years preceding menopause. Because of this estrogen dominance, this is a good time to be aware of xenoestrogens we are increasingly exposed to nowadays (for more on this see my post on endocrine disruptors).
The age at which a woman will reach menopause, as well as the probability to go through menopause prematurely are known to have a strong genetic component, so find out when your mother did and you will have an idea of what to expect.


 RSS Feed
RSS Feed