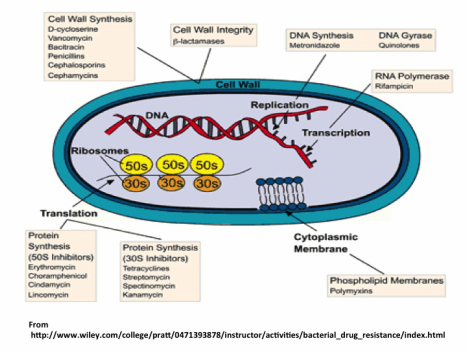
The way antibiotics work is by altering or inhibiting bacterial cell structures or processes that are essential for bacterial growth. These mechanisms and specific antibiotics for each are shown in the figure below showing a cell and its parts. The most common mechanism of action is by inhibiting the making of the cell wall (penicillins and cephalosporins) by targeting its major structural component, the peptidoglycan layer. Other antibiotics affect the structure of the cellular membrane, whereas some act by inhibiting protein synthesis (tetracyclines, macrolides and clindamycin), synthesis of DNA or RNA (metronidazole and quinolones, rifampicin) or a metabolic pathway (sulfonamides). Antibiotics that kill bacteria (bactericidal) include the penicillin group that kills susceptible bacteria by inhibiting the synthesis of the bacterial peptidoglycan cell wall that provides the cell with rigidity.
Unfortunately, prescribing antibiotics is common practice in many countries even before evidence of a bacterial infection in the patient is available. In fact, antibiotics are the most overprescribed drugs. They work as anti-bacterial (also against fungi and parasites) agents but not for viral infections, such as colds or the flu. For some viral infections such as influenza, herpes, and HIV the drugs taken are called antivirals. A current public health problem is the emergence and spread of drug-resistant infections (check my previous post on this subject if you are interested).
Bacteria in food can also become resistant because of the use of antibiotics in animals. These resistant bacteria can contaminate meat and other animal products, as well as the environment when animal waste products spread to produce via contaminated water used for irrigation.
Because antibiotics act very quickly to kill MOST bacteria that cause infection (in about 24-48h) many people taking them are tempted to stop earlier than the prescribed full course (a week or 10 days sometimes). However, there will be remaining bacteria, and among these, the ones “selected” by the antibiotic and resistant to it will be enriched and will survive and reproduce. In low resources settings, it is common to save the leftover antibiotics and take them later on if the infection comes back, risking treatment failure due to expired or damaged antibiotics, as well as emergence and spread of drug resistance.


 RSS Feed
RSS Feed