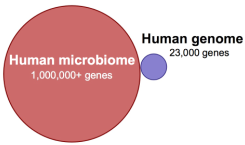
 From http://laughingsquid.com/asapscience-explains-the-human-microbiome-the-microorganisms-that-share-space-with-the-human-body/ (a 3 min video and nice overview of what microbiomes are and do for you).
From http://laughingsquid.com/asapscience-explains-the-human-microbiome-the-microorganisms-that-share-space-with-the-human-body/ (a 3 min video and nice overview of what microbiomes are and do for you). About 2400 years ago, Hippocrates said: "All disease begins in the gut"
 From http://mpkb.org/home/pathogenesis/microbiota
From http://mpkb.org/home/pathogenesis/microbiota 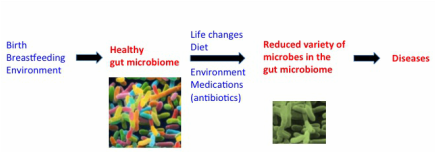

 RSS Feed
RSS Feed